


 Secure and encrypted payment processing
Secure and encrypted payment processing We ship to over 40 countries including the USA, UK, Europe, Australia and Japan
We ship to over 40 countries including the USA, UK, Europe, Australia and Japan Guaranteed refund or reship if you haven't received your order
Guaranteed refund or reship if you haven't received your orderamlodipine - an antagonist of calcium ions (a blocker of slow calcium channels), blocks the transmembrane current of calcium ions to the smooth muscle cells of the myocardium and blood vessels. the mechanism of the antihypertensive effect of amlodipine is due to the direct relaxing effect on the smooth muscles of blood vessels. the antianginal effect of amlodipine is due to two mechanisms:
In patients with hypertension, taking amlodipine once a day provides a clinically significant decrease in blood pressure over 24 hours. Due to the slow onset of action of amlodipine, there is no sharp decrease in blood pressure.
In patients with angina pectoris, amlodipine lengthens the total exercise time, the time before the onset of angina pectoris and the time before the onset of significant ST segment depression, and also reduces the frequency of angina attacks and reduces the need for nitroglycerin.
Amlodipine does not cause unwanted metabolic effects or changes in the level of lipids in the blood plasma, so it can be used in patients with AD, diabetes and gout.
Bisoprolol - selective β blocker1-adrenoreceptors, without ICA, as well as without pronounced membrane-stabilizing properties.
Blocks β1-adrenoreceptors and reduces the effect of catecholamines on them. It has antihypertensive and antianginal effects.
The mechanism of antihypertensive action is carried out by reducing cardiac output, sympathetic stimulation of peripheral vessels and renin release by the kidneys.
Antianginal action associated with β blockade1-adrenoreceptors, which leads to a decrease in myocardial oxygen demand through negative chronotropic and inotropic effects. Thus, bisoprolol eliminates or reduces the severity of symptoms of ischemia.
The maximum effect appears 3-4 hours after oral administration. Usually the maximum hypotensive effect is achieved after 2 weeks of use.
Pharmacokinetics
Amlodipine. After oral administration in therapeutic doses, amlodipine is well absorbed and reaches Cmax in the blood 6-12 hours after application. Eating does not affect the bioavailability of amlodipine. Absolute bioavailability is 64–80%. Distribution volume - about 21 l / kg. In vitro studies have shown that about 93–98% of circulating amlodipine binds to plasma proteins.
Amlodipine is metabolized in the liver with the formation of inactive metabolites, 10% of the drug is excreted unchanged in the urine and 60% in the form of metabolites, 20-25% with feces.
T½ from blood plasma is about 35-50 hours, which allows you to take the drug 1 time per day.
Bisoprolol is almost completely (up to 90%) absorbed in the digestive tract. The effect of the first passage through the liver is slightly expressed (about 10%), the absolute bioavailability is about 90%. T½ from blood plasma is 10-12 hours, this provides a therapeutic effect for 24 hours after a single dose of the daily dose.
Distribution volume - 3,5 l / kg. Binding to plasma proteins - 30%.
Bisoprolol is excreted in two ways. 50% is metabolized in the liver to inactive metabolites that are excreted by the kidneys. The remaining 50% is excreted by the kidneys unchanged. Active metabolites are not formed in the human body.
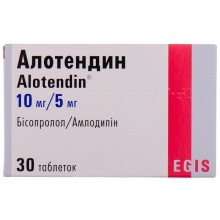
Ag as monotherapy or in combination with other antihypertensive agents.
Chronic stable angina pectoris - as monotherapy or in combination with other antianginal drugs.
As a replacement therapy in patients in whom blood pressure and / or stable angina are adequately controlled by the simultaneous use of amlodipine and bisoprolol in the same doses.
The recommended daily dose is 1 tablet of the appropriate dosage, which is desirable to take in the morning, regardless of food intake, without chewing.
The maximum daily dose is 1 tablet of Alotendin 10 mg / 10 mg / day.
The dosage range of the drug allows you to flexibly select the ratio of components depending on clinical need.
Treatment should not be stopped suddenly, as this can lead to a temporary worsening of the clinical condition. This is especially true for patients with coronary heart disease. A gradual dose reduction is recommended.
Impaired liver and kidney function. With liver failure, the elimination of amlodipine slows down. There are no special recommendations regarding the dosage of amlodipine, therefore, the drug should be prescribed with caution in patients with impaired liver function. In severe liver failure, the daily dose of bisoprolol should not exceed 10 mg.
In patients with mild or moderate renal failure, there is no need to change the dosage. In severe renal failure (creatinine clearance of 20 ml / min), the daily dose of bisoprolol should not exceed 10 mg.
Elderly patients can be prescribed the usual dose of the drug.
The combined drug amlodipine / bisoprolol is not recommended for children under 18 years of age due to a lack of data regarding the safety and effectiveness of the drug.
For amlodipine / bisoprolol tablets: hypersensitivity to amlodipine, dihydropyridine derivatives, bisoprolol and / or any excipient.
For amlodipine:
For bisoprolol:
Adverse reactions can be caused by each of the components of the drug.
When using amlodipine, the following adverse reactions often occur: headache, swelling (especially in the lower leg), increased fatigue, drowsiness, nausea, abdominal pain, hot flashes, palpitations, dizziness.
Laboratory tests: elevated liver enzymes.
From the cardiovascular system: tachycardia; arrhythmia (including bradycardia, ventricular tachycardia, and atrial fibrillation); myocardial infarction.
On the part of the blood and lymphatic system: leukopenia, thrombocytopenia, purpura.
From the nervous system: headache, dizziness, drowsiness, peripheral neuropathy, fainting, hypesthesia, paresthesia, taste disturbances, tremors, hypertonicity, peripheral neuropathy.
From the side of the organ of vision: visual impairment (including diplopia).
From the side of the organ of hearing and the maze: ringing in the ears.
From the respiratory system: shortness of breath, cough, rhinitis.
From the digestive system: nausea, abdominal pain, dyspepsia, gingival hyperplasia, pancreatitis, dry mouth, gastrointestinal motility; gastritis; vomiting
From the kidneys and urinary system: frequent urination, impaired urination, nocturia.
On the part of the skin and subcutaneous tissues: increased sweating, alopecia, discoloration of the skin; allergic reactions, rash, itching, angioedema, erythema multiforme exudative; hives; purpura, discoloration of the skin, exanthema; angioedema, erythema multiforme, exfoliative dermatitis, Stevens-Johnson syndrome, Quincke edema, photosensitivity.
From the musculoskeletal system: arthralgia, myalgia, back pain, muscle cramps; swelling of the legs.
Metabolic disorders: hyperglycemia.
From the vascular system: flushing; vasculitis; arterial hypotension.
General disorders: edema, peripheral edema, increased fatigue; fatigue, asthenia, increase or decrease in body weight.
From the hepatobiliary system: cholestasis, jaundice, hepatitis; increased levels of liver enzymes (most often associated with cholestasis).
From the reproductive system: impotence, gynecomastia.
Mental disorders: depression, mood changes (including anxiety), insomnia, confusion.
Similar to other calcium antagonists, adverse reactions such as myocardial infarction, arrhythmia (including ventricular tachycardia and atrial fibrillation, angina pectoris) have been reported, but it is almost impossible to find out if they are associated with the underlying disease.
General disorders and conditions at the injection site: edema, fatigue, asthenia, chest pain, pain, malaise.
Research: increase or decrease in body weight; exceptional cases of extrapyramidal syndrome have been reported.
Reported suspected adverse reactions. Reporting suspected adverse reactions after drug registration is important. This allows continuous monitoring of the relationship between the benefits and the risks associated with the use of this drug. The doctor should report any suspected adverse reactions in accordance with legal requirements.
When using bisoprolol
From the cardiovascular system: bradycardia (in patients with chronic heart failure); violation of AV conduction, increased manifestations of heart failure; signs of worsening heart failure (in patients with chronic heart failure); bradycardia (in patients with hypertension or coronary artery disease), signs of worsening heart failure (in patients with hypertension or coronary artery disease).
From the nervous system: headache *; dizziness*; sleep disturbance; fainting.
From the side of the organ of vision: decreased secretion of lacrimal fluid, which must be considered by patients who use contact lenses; conjunctivitis.
On the part of the organ of hearing and the maze: hearing impairment.
On the part of the respiratory system: bronchospasm (especially in patients with AD or obstructive bronchial diseases in the anamnesis); allergic rhinitis.
From the digestive tract: nausea, vomiting, diarrhea, constipation.
On the part of the skin and subcutaneous tissues: allergic reactions, rash, itching, alopecia, psoriatic rash.
From the musculoskeletal system: muscle weakness, cramps.
Metabolic disorders: increased levels of TG.
From the vascular system: worsening of peripheral circulation (sensation of coldness in the limbs), arterial hypotension (especially in patients with heart failure).
General disorders: fatigue, exhaustion.
On the part of the hepatobiliary system: increased levels of liver enzymes (AlAT, AsAT), hepatitis.
From the reproductive system: impotence.
Mental disorders: depression nightmares, hallucinations, sleep disturbance.
Laboratory indicators: an increase in the level of TG in the blood.
General disorders: asthenia (in patients with chronic heart failure), increased fatigue *; asthenia (in patients with hypertension or ischemic heart disease).
* Symptoms such as dizziness, headache, fatigue, fatigue, are typical for the start of treatment and often disappear within 1-2 weeks.
In case of side effects or adverse reactions, the patient should immediately inform the doctor.
For amlodipine
The safety and effectiveness of amlodipine in hypertensive crisis have not been evaluated.
Patients with heart failure. In this category of patients, amlodipine should be used with caution. In a long, placebo-controlled study in patients with severe heart failure (NYHA class III and IV), amlodipine was associated with a higher incidence of pulmonary edema compared with placebo. In patients with congestive heart failure, calcium channel blockers, including amlodipine, should be used with caution, as they may increase the risk of future cardiovascular events and deaths.
Patients with impaired liver function. T½ amlodipine and AUC parameters are higher in patients with impaired liver function; there are no recommendations for dosing the drug. Therefore, this category of patients should begin to use the drug with a low dose. Caution should be exercised both at the beginning of the use of the drug, and when increasing the dose. Patients with severe hepatic impairment may require slow dose selection and close monitoring of the patients condition.
Elderly patients. Increase the dose of the drug in this category of patients with caution.
Patients with renal failure. In this category of patients, usual doses of the drug should be used. Changes in the concentration of amlodipine in blood plasma do not correlate with the degree of impaired renal function. Amlodipine is not excreted by dialysis.
Amlodipine does not affect laboratory results.
It is not recommended to use amlodipine with grapefruit or grapefruit juice, as in some patients the bioavailability may be increased, which will lead to an increase in the hypotensive effect of the drug.
Fertility. Reversible biochemical changes in the sperm head in some patients have been reported with calcium channel blockers. There is insufficient clinical information regarding the potential effects of amlodipine on fertility.
For bisoprolol
Patients with coronary artery disease should not be discontinued suddenly if necessary, as this can lead to a transient worsening of the condition. Bisoprolol should be prescribed with caution to patients with hypertension or angina pectoris, which is associated with heart failure.
Initiation and discontinuation of bisoprolol treatment requires regular monitoring.
Bisoprolol should be used with caution in the following conditions:
The drug contains an active substance that gives positive results with anti-doping control.
During pregnancy and breastfeeding
For amlodipine
The safety of amlodipine during pregnancy has not been established. The use of amlodipine during pregnancy is recommended only in cases where there is no safer alternative, and the risk associated with the disease itself exceeds the possible harm from treatment to the mother and fetus.
In animal studies with high doses, reproductive toxicity was noted.
The period of breastfeeding. It is not known whether amlodipine passes into breast milk. When deciding whether to continue breastfeeding or on the use of amlodipine, it is necessary to evaluate the benefits of breastfeeding for the baby and the benefits of using the drug for the mother.
For bisoprolol
Bisoprolol has pharmacological properties that can cause harmful effects on pregnancy and / or the development of the fetus / newborn.
Blockers of β-adrenergic receptors reduce placental perfusion, which causes stunting, fetal freezing, spontaneous abortion, and early delivery. The fetus and newborn may develop hypoglycemia and bradycardia. If treatment with β-adrenoreceptor blockers is necessary, selective β blockers prevail1-adrenoreceptors.
Bisoprolol should not be used during pregnancy if there is no clear indication for this. If treatment with bisoprolol is defined as necessary, monitoring of uteroplacental circulation and fetal growth should be monitored. In the event of a negative effect on pregnancy or the fetus, the issue of alternative treatment should be addressed. Newborns should be closely monitored. Hypoglycemia and bradycardia can usually be expected in the first 3 days.
Breastfeeding. It is not known whether the drug passes into breast milk and, if it penetrates, whether bisoprolol can harm the baby. In this regard, the use of amlodipine / bisoprolol tablets during lactation is not recommended.
Children. Alotendine is not recommended for use in children.
Bisoprolol. There are no clinical data on the efficacy and safety of the drug in children.
The ability to influence the reaction rate when driving vehicles and working with other mechanisms. Given the different individual response of the patient, the ability to influence the reaction rate when driving vehicles or working with other mechanisms may be impaired, especially at the beginning of treatment, when changing treatment.
Amlodipine
Preparations with which simultaneous use requires caution: thiazide diuretics, β-adrenoreceptor blockers, prolonged nitrates, sublingual nitroglycerin, NSAIDs, antibiotics and oral hypoglycemic drugs.
The simultaneous use of amlodipine with digoxin does not lead to a change in the concentration of digoxin in the blood plasma and does not affect its renal clearance.
The simultaneous use of amlodipine with cimetidine does not affect the pharmacokinetics of amlodipine.
The simultaneous use of amlodipine with warfarin does not significantly affect prothrombin time.
The effect of other drugs on amlodipine. CYP 3A4 Inhibitors. The simultaneous use of amlodipine and potent or moderate-acting CYP 3A4 inhibitors (protease inhibitors, azole antifungal agents, macrolides such as erythromycin or clarithromycin, verapamil or diltiazem) can lead to a significant increase in amlodipine exposure, which can increase the risk of hypotension. The clinical significance of such changes may be more pronounced in elderly patients. Clinical monitoring of the patients condition and dose selection may be required.
It is not recommended to simultaneously use amlodipine and consume grapefruit or grapefruit juice, since in some patients the bioavailability of amlodipine may increase, which, in turn, leads to an increase in the hypotensive effect.
Inductors CYP 3A4. There is no information on the effect of CYP 3A4 inducers on amlodipine. The simultaneous use of amlodipine and substances that are inducers of CYP 3A4 (for example, rifampicin, St. Johns wort) can lead to a decrease in the concentration of amlodipine in blood plasma, therefore, such combinations should be used with caution.
Dantrolene (infusion). In animals, fatal ventricular fibrillation and cardiovascular collapse, which were associated with hyperkalemia, were observed after the use of verapamil and iv dantrolene. Due to the risk of developing hyperkalemia, it is recommended to avoid the use of calcium channel blockers, such as amlodipine, in patients prone to malignant hyperthermia and in the treatment of malignant hyperthermia.
The effect of amlodipine on other drugs. The hypotensive effect of amlodipine potentiates the hypotensive effect of other antihypertensive agents.
Tacrolimus. There is a risk of increased levels of tacrolimus in the blood while using amlodipine, but the pharmacokinetic mechanism of this interaction has not been fully established. To avoid the toxicity of tacrolimus while the use of amlodipine, regular monitoring of the level of tacrolimus in the blood and, if necessary, dose adjustment are necessary.
Cyclosporin. Studies of the interactions of cyclosporine and amlodipine in healthy volunteers or in other groups have not been carried out, except for use in patients with a transplanted kidney, in which an increase in the residual concentration of cyclosporine is noted (on average by 0–40%). For patients with a transplanted kidney who are using amlodipine, consideration should be given to monitoring cyclosporin concentrations and, if necessary, lowering the dose of cyclosporin.
Simvastatin. The simultaneous use of multiple doses of amlodipine 10 mg and simvastatin at a dose of 80 mg led to an increase in the exposure of simvastatin by 77% compared with the use of simvastatin alone.For patients who use amlodipine, the dose of simvastatin should be limited to 20 mg / day.
Clinical studies of drug interactions have shown that amlodipine does not affect the pharmacokinetics of atorvastatin, digoxin, and warfarin.
For bisoprolol
Concomitant administration is not recommended. Calcium antagonists (verapamil and, to a lesser extent, diltiazem) adversely affect contraction, AV conductivity and blood pressure. The administration of verapamil to patients who use β-adrenergic receptor blockers can lead to significant arterial hypotension and AV block.
Hypertensive drugs of central action (clonidine, methyldopa, moxonidine, rilmenidine): the simultaneous administration of these drugs can lead to a slowdown in heart rate, cardiac output and vasodilation. Sudden drug withdrawal may increase the risk of withdrawal syndrome in the form of hypertension.
Drugs, the simultaneous use of which requires caution. Calcium antagonists such as dihydropyridine, such as nifedipine: due to an increased risk of arterial hypotension and a risk of developing heart failure.
Class I antiarrhythmic drugs (e.g., disopyramide, quinidine, lidocaine, phenytoin, flecainide, propafenone): due to an increase in the negative effect on the inotropic function of the myocardium, AV conductivity.
Class III antiarrhythmic drugs (e.g., amiodarone): due to increased effects on AV conduction.
Parasympathomimetics: with simultaneous use, it can cause an increase in AV conduction time and thereby increase the risk of bradycardia.
Topical products containing β-adrenergic blockers (eye drops for the treatment of glaucoma): may complement the systemic effect of bisoprolol.
Insulin and oral antidiabetic agents: increased hypoglycemic effect. Blockade of β-arenoreceptors may mask the symptoms of hypoglycemia.
Cardiac glycosides: decreased heart rate, prolonged AV conduction.
NSAIDs: decrease in antihypertensive effect.
β-Sympathomimetics (isoprenaline, dobutamine): a combination with bisoprolol can reduce the effects of both drugs.
Sympathomimetics that activate α- and β-adrenergic receptors (e.g. epinephrine, norepinephrine): increase blood pressure. Such an interaction is more likely when using non-selective β-adrenergic receptor blockers.
Ergotamine derivatives: exacerbation of peripheral circulation disorders.
Tricyclic antidepressants, barbiturates, phenothiazines, and other antihypertensive drugs: increase the risk of arterial hypotension.
Means for inhalation anesthesia, carbohydrate derivatives (chloroform, cyclopropane, halotane, methoxyflurane), while using β-adrenergic receptor blockers, increase the risk of inhibition of myocardial function and the development of antihypertensive reactions.
The action of non-depolarizing neuromuscular transmission blockers can be enhanced and lengthened under the influence of β-adrenergic receptor blockers.
Drugs, the simultaneous use of which requires discussion. Mefloquine increases the risk of bradycardia.
MAO inhibitors (with the exception of MAO-B inhibitors): increased hypotensive effect of β-adrenoreceptor blockers, as well as increased risk of hypertensive crisis.
Rifampicin: possible slight decrease in T½ bisoprolol in connection with the effect on the metabolism of the drug liver enzymes. But dose adjustment is not required.
For amlodipine
Experience with deliberate overdose is limited.
Overdose symptoms: the available information suggests that a significant overdose of amlodipine will lead to excessive peripheral vasodilation and, possibly, reflex tachycardia. Significant and possibly prolonged systemic arterial hypotension has been reported, including fatal shock.
Treatment: clinically significant arterial hypotension due to an overdose of amlodipine requires active support of the cardiovascular system, including frequent monitoring of heart function and respiration, raising the lower extremities, monitoring the volume of circulating fluid and urination.
To restore vascular tone and blood pressure, vasoconstrictor drugs can be used, making sure that there are no contraindications to their use. The use of calcium gluconate IV can be effective for leveling the effects of calcium channel blockade.
In some cases, gastric lavage may be effective. The use of activated carbon in healthy volunteers within 2 hours after the administration of 10 mg of amlodipine significantly reduced its absorption.
Since amlodipine is significantly bound to proteins, the effect of dialysis is negligible.
For bisoprolol
Common symptoms of an overdose are bradycardia, arterial hypotension, acute heart failure, bronchospasm, hypoglycemia. There is wide variability in individual sensitivity to a single high dose of bisoprolol; heart failure patients may be more sensitive to the drug.
In case of overdose, consult a doctor immediately.
Depending on the degree of overdose, discontinue treatment with the drug and conduct supportive and symptomatic therapy. There is limited evidence that bisoprolol is difficult to dialysis.
With bradycardia: administration of atropine. If there is no reaction, isoprenaline or another drug with a positive chronotropic effect should be administered with caution. In exceptional cases, introduce an artificial pacemaker.
With arterial hypotension: taking vasoconstrictor drugs, iv administration of glucagon.
With AV blockade of the II and III degree: infusion of isoprenaline; if necessary - pacemaker.
With exacerbation of chronic heart failure: the introduction of diuretics and vasodilators.
With bronchospasm: bronchodilators (e.g. isoprenaline), β2-adrenomimetics and / or aminophylline.
With hypoglycemia: iv administration of glucose.
At a temperature not exceeding 30 ° C.